Asia Pacific faces a growing prevalence of chronic diseases, or non-communicable diseases (NCDs), prompted by the rise in ageing populations. In fact, 55% of all deaths in Southeast Asia are due to NCDs. On top of having to fight infectious diseases such as Covid-19, NCDs pose a significant burden on health systems in the region.
A data-driven approach to managing the health of patient populations with NCDs can significantly alleviate this burden. Biospectrum Asia spoke to Farhana Nakhooda, Senior Vice President, Asia Pacific at Health Catalyst, who shared additional insight on the importance of population health management in Asia-Pacific, challenges faced by health systems in managing population health and the opportunity for data and analytics to enhance population health management, improving patient outcomes, and reducing healthcare expenses.
Chronic diseases are one of the biggest healthcare concerns in the world, claiming an estimated 40 million lives every year, 8.5 million of whom reside in Asia. In Asia Pacific, cardiovascular diseases, diabetes, cancer, and chronic respiratory conditions are among the most common chronic diseases. This is primarily being driven by ageing populations and poor lifestyle choices such as the lack of physical activity and consumption of tobacco and alcohol.
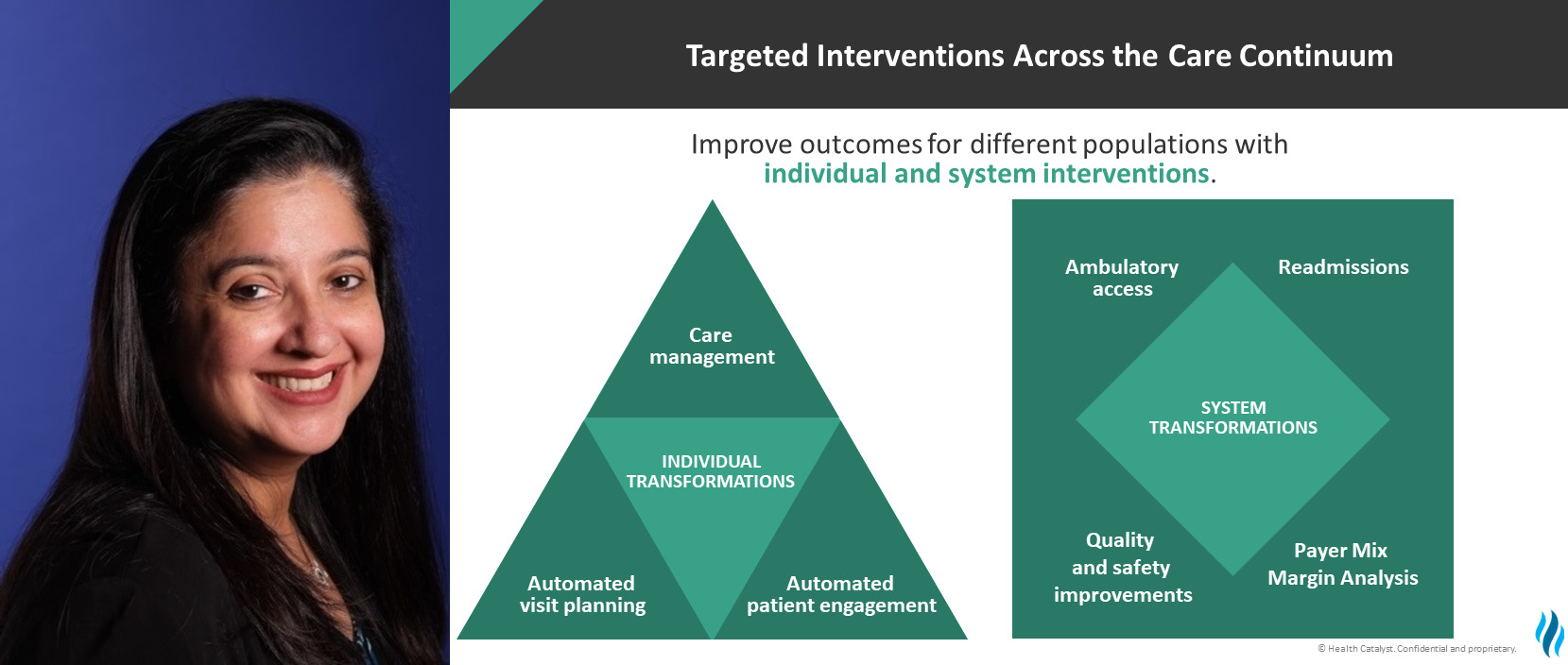
Healthcare spending typically follows the 80/20 rule, where 80% of healthcare costs are incurred by 20% of the population – usually made up of cohorts suffering from complex chronic conditions. The increasing incidence of chronic diseases places a strain on health systems in the region, particularly for developing countries that are already grappling with inadequate financial and human resources, poor service delivery, and weak information systems. A well-thought-out population health management strategy can help to alleviate some of these burdens by actively identifying, enrolling, managing, and monitoring individuals that are likely to fall into this 20% of the population. This also involves looking at high-risk patients who are trending towards, and are likely to end up with, a chronic disease and putting them on preventative programs. Finally, the rest of the population who are healthy today need to ensure they are going for regular health screenings to minimize any chances of ending up in the high-risk group. This holistic approach to population health management ensures that the health of the entire population is looked after, while programs are tailored based on individual healthcare needs.
Consider a group of patients with diabetes from diverse socio-economic backgrounds – providing a one-size-fits-all care management approach may not effectively improve health outcomes of this group, as individuals may require different levels of attention and care. For example, accessibility to healthy food, stable employment, proper housing, and family support are just a few key social factors that can impact whether patients will get better or worse. Being able to expertly manage these nuances are critical in both improving health outcomes and reducing healthcare costs.
Population health management accounts for factors that make up the complete picture of individual and group health, including demographics, lifestyle, and social background, among others. This leads to a more tailored delivery of care, which improves patient outcomes and allows for a more efficient allocation of healthcare resources.
The biggest challenge is delivering and improving care for people with chronic conditions, while remaining vigilant against infectious diseases. Many healthcare providers today are already under immense pressure fighting against infectious diseases, such as Covid-19, which has severely disrupted the treatment of chronic diseases.
A significant amount of healthcare resources is required for the effective management of chronic diseases, including detection, screening, treatment, and providing access to palliative care. Many health systems lack the resources to keep up with these requirements – in Asia Pacific, for instance, there aren’t enough doctors to keep up with this demand, with many teaching patients to self-manage conditions and minimize hospital visits.
Another major challenge is cost and affordability. Managing chronic diseases is costly for both healthcare providers and patients. Take the case of diabetes – the cost of care for a single patient amounts to a staggering average of US$16,752 per year. This has the potential to impact livelihoods. A study in Southeast Asia revealed that 48% of cancer patients experienced financial catastrophe, due to the out-of-pocket expenses required for treatment. In countries where access to healthcare funding is limited, long-term treatment can even push people over the poverty line.
In addition, one of the most important aspects around effective preventative and proactive healthcare is an understanding of behavioural science. Most people who are overweight know that they need to lose weight and that their weight can lead to diabetes and other chronic conditions. Similarly, most people who are smokers know that smoking will decrease life expectancy. However, many continue to eat unhealthily and smoke. This can be attributed to a number of reasons, including stressful lifestyles, depression, loneliness, among others, which all impact one’s mental state. The ability to understand and influence people to change their behaviour is a science and art in itself.
Lastly, the lack of timely access to accurate, near real-time data makes it challenging to actively identify at-risk cohorts and manage populations. Care teams often make decisions based on outdated data and have limited ways to measure the effectiveness of their programs. Laying the foundation for care teams so they can have access to the right data at the appropriate time to measure success of their population health strategies is critical.
There is immense opportunity for data and analytics to lift the burden of chronic diseases on Asia Pacific’s health systems and also keep the rest of the population from becoming chronically ill. With access to accurate and real-time data, healthcare providers will be better equipped to plan, allocate resources, and implement appropriate intervention strategies for patient populations.
Data and analytics can provide greater transparency into the population health journey by understanding what goes on beyond the four walls of a hospital. For example, in the case of diabetes, social determinants such as economic stability, education, social and community context, all impact the effectiveness of the self-management of diabetes. Having access to this data can empower healthcare providers to identify barriers to diabetes care, and subsequently design a program that suits the patients’ social background. This approach helped a healthcare provider in the US to reduce patient follow-up visits by 19%, as patients feel more confident and well-equipped to manage their diabetes. Leveraging data and analytics, the hospital was able to understand individual barriers, such as lack of knowledge, poor transportation, or affordability of medication, and worked to make diabetes care more accessible to each patient. The same approach can be applied to most types of chronic conditions.
Data can provide a more complete view across the patient care continuum within and outside of the health system, offering greater insight into the environments in which patients live, work, and play. This helps providers to prevent people from becoming chronically ill, personalise care, and help patients succeed in managing their own chronic conditions. This is exceptionally important as health systems in Asia Pacific start looking at transitioning to value-based care, where success hinges on improved patient outcomes rather than just the volume of patients cared for. As Asia Pacific continues to grapple with its ageing populations and high incidences of chronic diseases, this data-driven approach can create a more sustainable path to managing population health.
Hithaishi C Bhaskar




